Randomized clinical trials (RCT) are imperative for testing novel cancer therapies and advancing the science of cancer care. Exclusion criteria are employed to minimize toxicity and maximize benefit. However, the selection process introduces a deviation between enrolled patients (pts) and the real world population. Estimating how much the selected population deviates from the MM cohort at large may increase inclusiveness and could help define barriers to recruiting to MM studies.
There has been significant advancement in treating Multiple Myeloma (MM) during the last decade. Over 16 FDA-approved anti-myeloma regimens are now available. We selected the recent 6 RCTs (ASPIRE, TOURMALNE-MM01, ELOQUENT-2, ENDEAVOR, POLLUX and CASTOR studies) which were pharma-sponsored landmark trials that provided the basis for FDA approval of a new agent or established a new indication for formerly FDA-approved drug. We intended to quantify the gap between the trial population and real world by examining the eligibility criteria of these trials compared against a single institution database.
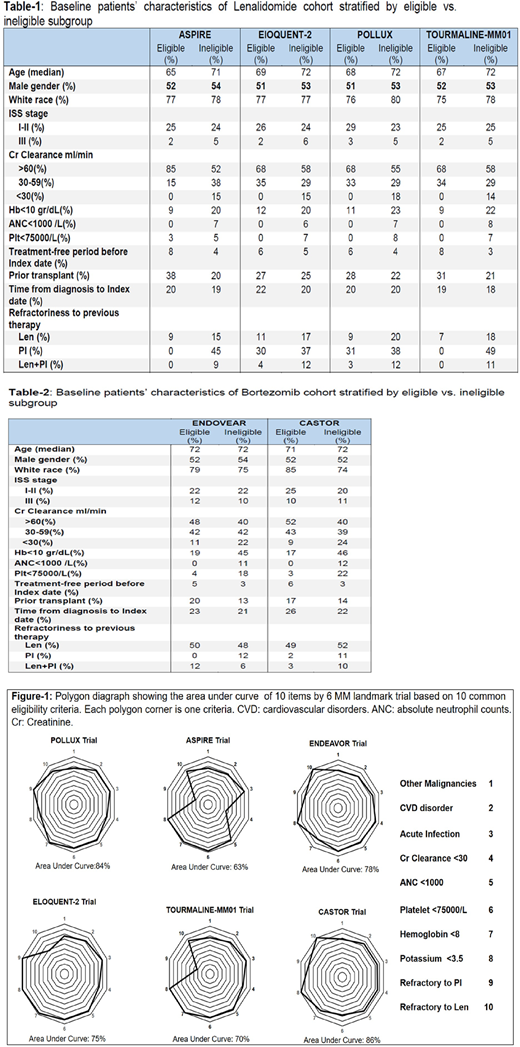
Methods: Pts with relapsed MM initiating second or later line of therapy containing lenalidomide (Len) or bortezomib (Bor) were identified retrospectively. The 3-week period before the index treatment date was used to apply the eligibility criteria of the mentioned 6 trials. Pts who received Len-containing regimens were tested as to be enrolled on trials with Len/Dex control arm (ASPIRE, TOURMALINE-MM1, POLLUX, and ELOQUENT-2) and pts who had Bor-containing regimens were reviewed to be enrolled on Bor/Dex trials (CASTOR and ENDEAVOR). Pts were classified as "Trial eligible" or "Trial ineligible", accordingly. Pts were followed up longitudinally from the index treatment date until death, loss to follow-up, or the end of the study period (Jan, 2018). Ten frequently used eligibility criteria were studied (Fig-1). History of other malignancies, except skin and prostate cancer, was defined as any cancer requiring therapy other than anti-myeloma regimen in the 3 years prior to the index treatment date. Current infection referred to the use of any medication other than acyclovir, ciprofloxacin or Bactrim. Shoelace algorithm was used to calculate area under the curve of the polygon graphs.
Results: 516 pts were studied between 2010 and 2018; 153 pts were excluded due to missing values, while 224 and 136 pts were treated with Len-containing and Bor-containing regimens, respectively. Overall, the trial-eligible cohort was more likely to have autologous stem cell transplant and to have had longer treatment-free period before index treatment date (p-value: 0.012). There was a substantial variation in the ineligibility rate for these 6 RCTs among the study population (Fig-1). The most common items that excluded a patient from a RCT were: Other malignancies, current infection and renal dysfunction. Within the Len cohort the trial-specific Glomerular Filtration Rate (GFR) threshold for renal function was highest in ASPIRE trial (Cr clearance> 50 ml/min) causing high rate of exclusion (29% vs. 8% in other trials). Only TOURMOULINE-MM01 and ASPIRE trials had bor-refractory status as the exclusion criteria leading to 36% ineligibility rate. The differences between the trial-eligible and trial-ineligible pts stratified by trial are listed in Table-1 and 2 for trials with Len and Bor as the control arms, respectively. The median follow-up for the Len and Bor cohort was 31 and 30 months, respectively. The trial-ineligible pts had significantly worse OS (2-year survival rate 69% vs. 82%, P-value: 0.001) and 43% higher chance of death (hazard ratio 1.43, 90% confidence interval (CI): 1.08-2.02) compared with trail-eligible cohort.
Conclusion: Here we assessed the eligibility criteria of 6 landmark MM studies and showed that ineligibility rates were quite different amongst these trials suggesting significant limitations in cross-trial comparison. Furthermore, trial-eligibility per se was associated with improved survival. We therefore proposed a quantitative deviation score calibrating the generalizability of the results of these trials to a single institution cohort. Such a tool can lead to efforts to broaden eligibility criteria and possibly narrow the gap between reported clinical trial efficacy and the observed effectiveness in real-world MM pts.
de Lima:Kadmon: Other: Personal Fees, Advisory board; Incyte: Other: Personal Fees, advisory board; BMS: Other: Personal Fees, advisory board; Celgene: Research Funding; Pfizer: Other: Personal fees, advisory board, Research Funding. Malek:Medpacto: Research Funding; Takeda: Other: Advisory board , Speakers Bureau; Bluespark: Research Funding; Cumberland: Research Funding; Sanofi: Other: Advisory board; Janssen: Other: Advisory board, Speakers Bureau; Clegene: Other: Advisory board , Speakers Bureau; Amgen: Honoraria.
Author notes
Asterisk with author names denotes non-ASH members.